5 timeless habits for better health

What are the symptoms of prostate cancer?

Is your breakfast cereal healthy?

When pain signals an emergency: Symptoms you should never ignore

Does exercise give you energy?

Acupuncture for pain relief: How it works and what to expect

How to avoid jet lag: Tips for staying alert when you travel

Biofeedback therapy: How it works and how it can help relieve pain

Best vitamins and minerals for energy

Should you take probiotics with antibiotics?
Medications Archive
Articles
FDA approves new migraine medication
Research we're watching
If you suffer from migraine headaches, there's a new option available to relieve your pain. In October 2019, the FDA approved lasmiditan (Reyvow) to treat migraine pain in adults. Taken as a pill, it works for migraines either with or without an aura (a visual disturbance within the hour before migraine pain starts). Lasmiditan is not designed to prevent migraines. Lasmiditan is the first migraine treatment in a class of drugs known as serotonin (5-HT) 1F receptor agonists. In studies, researchers found that it could relieve pain and other migraine symptoms within two hours.
Migraines affect an estimated 28 million women in the United States, according to the American Migraine Foundation, and the World Health Organization ranks them among the top 10 disabling conditions. Pain and other symptoms, which may include nausea, sensitivity to light and temporary vision changes, result in lost work days, reduced productivity, and diminished quality of life for many people.
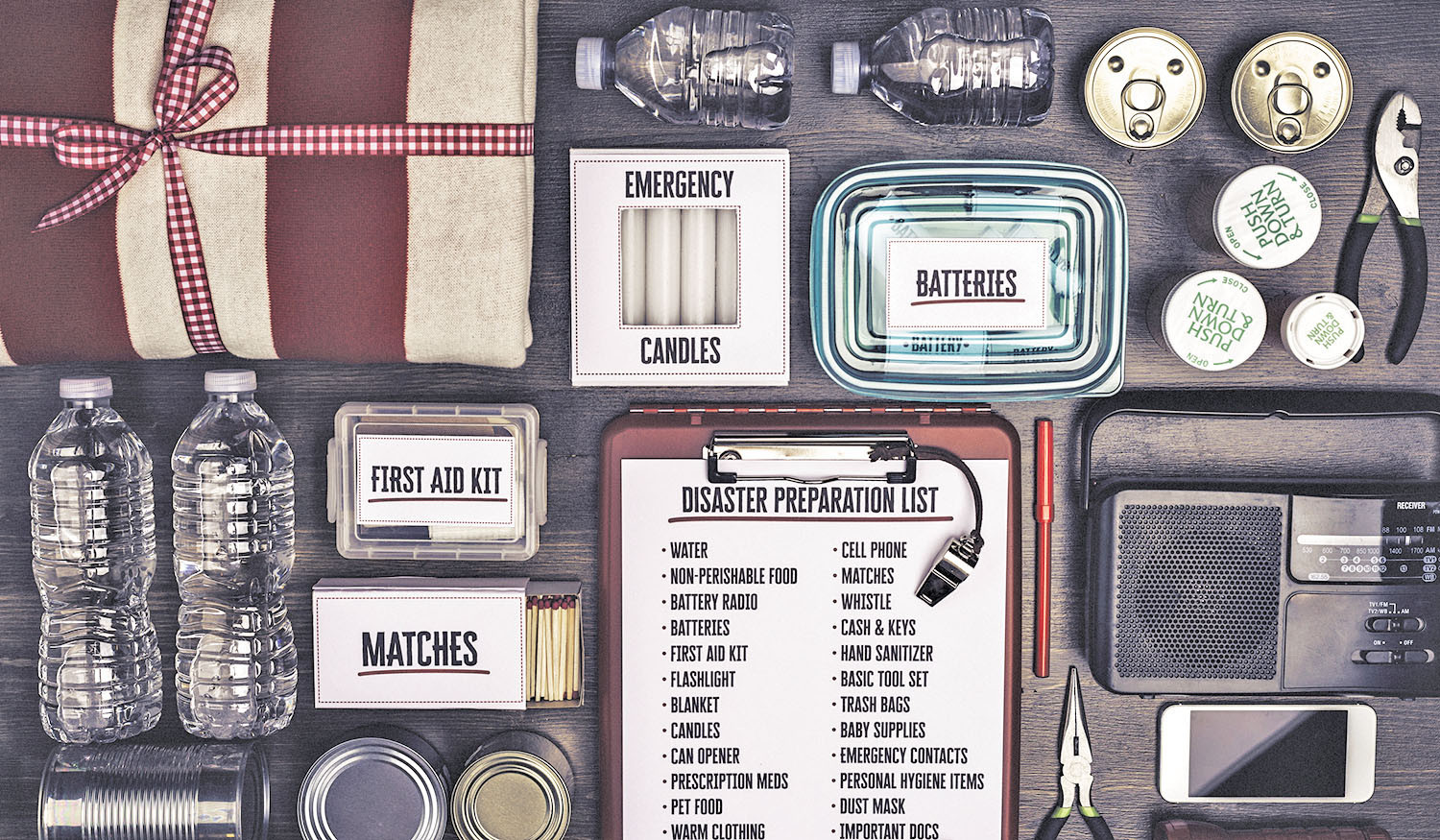
Be ready for emergencies
Here are 10 ways to safeguard your life (and health) when an emergency or disaster strikes.
Natural disasters and other kinds of emergencies can strike anywhere and often with little warning. Yet, new data from the University of Michigan National Poll on Healthy Aging show that most adults ages 50 to 80 are ill-prepared for severe weather, long-term power outages, or other emergency situations.
"Older adults should take the time to focus on how they will cope and manage with an emergency," says Dr. Howard LeWine, assistant professor of medicine at Harvard Medical School and editor-in-chief of this newsletter. "A small effort now can protect their health and well-being when an emergency does occur."
Can I do anything to prevent osteoporosis?
Ask the doctors
Q. I know that osteoporosis is linked to hereditary factors that I can't change. But are there things I can do to reduce my risk?
A. It's true that many risk factors for osteoporosis, such as your sex, age, and genes, are not things you can change. But there are things you can do to improve your bone health. This includes adopting a healthy diet that is rich in calcium and getting enough vitamin D, which can help maintain and improve bone health. Regular exercise can also help strengthen your bones or prevent bone loss. In particular, activities that put stress on your bones, such as jumping, running, and weight-bearing exercises, can stimulate bone cells to produce proteins that bolster bone strength. In children, these activities can actually increase bone density. While adults don't gain the same degree of benefit that kids do, exercise can still have moderate effects on bone, helping to maintain strength that might otherwise be lost. To further protect bone health, cut down on unhealthy habits, such as smoking or drinking excess amounts of alcohol. If you have risk factors for osteoporosis, you might also want to talk to your doctor about whether any of your medications might be harming your bone health.
Hair thinning? Get to the root of the problem
Bad mix: Blood thinners and NSAIDs
Image: Anita_Bonita/Getty Images |
Take the lowest dose of NSAIDs and stop using them as soon as possible.
Blood thinners are usually given to people at risk for developing blood clots from conditions, such as abnormal heart rhythms. Use of these lifesaving medications requires caution with other drugs, especially painkillers called nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil) or naproxen (Aleve). But plenty of people take the risk to relieve aches and pains. "Many of the patients who need blood thinners are older and therefore at risk for arthritis, so it's not infrequent for a patient to be on both a blood thinner and an NSAID," says cardiologist Dr. Deepak L. Bhatt, a Harvard Medical School professor.
Season of receiving: Use free services to stay independent
Nonprofit groups offer services that can help you age in place.
Image: © fstop123/Getty Images
The holidays are a time of giving, but they're also a time to put yourself on the receiving list and assess whether you should be taking advantage of free health-related services offered by nonprofit organizations. Services are widely available, often regardless of income. But you might not know they exist. "Most older adults aren't introduced to support services until they're hospitalized or they work with a case manager or social worker," explains Barbara Moscowitz, a geriatric social worker at Harvard-affiliated Massachusetts General Hospital. "You don't have to wait for such an event."
What's available
On the local level, you can often find free or low-cost dental clinics, emotional support groups, meal or grocery delivery services, transportation, in-home health evaluations, exercise classes, health education classes, home evaluations for fall prevention, companion programs, caregiver respite services, or programs to help you navigate difficult chronic health conditions and their treatment.
Advice about taking aspirin and statins after age 75
These drugs are mainstays for preventing heart disease. Are they safe and effective in older people?
Low-dose aspirin and statins are both common, inexpensive drugs that help prevent the two root causes of most heart attacks — blood clots and cholesterol-laden plaque clogging the arteries of the heart. In recent years, a number of studies have helped experts refine their advice as to who should or should not take these medications.
However, evidence-based advice for people in their mid-70s and beyond is a bit harder to come by. Historically, most drug trials have included only a small proportion of people 75 and older, in part because there are fewer people in that age demographic. Also, older people tend to have other chronic health conditions. As such, they may be more prone to drug side effects, making doctors reluctant to enroll them in clinical trials.
Who needs aspirin?
Age, family history, and other risk factors determine if daily aspirin can help prevent a heart attack or stroke.
For many of us, aspirin was the go-to medicine of our youth. Everything from headaches, colds, and general aches and pains were treated with two aspirin and a glass of water.
For decades, aspirin was widely believed to be a safe way to protect healthy adults from heart attacks and strokes. But over the past couple years, new research has questioned this premise and many doctors have already stopped prescribing aspirin for adults at low risk of cardiovascular disease.
High risk for breast cancer? You might benefit from preventive medication
Research we're watching
Women at high risk for breast cancer might benefit from taking medication to prevent the disease, says a new recommendation from the U.S. Preventive Services Task Force (USPSTF), a national group of experts. Medications such as tamoxifen (Nolvadex), raloxifene (Evista), and aromatase inhibitors have been shown to help prevent invasive, estrogen receptor-positive breast cancer, but they can cause serious side effects, such as other cancers and blood clots. For some women, the potential benefits of these drugs outweigh those risks. The USPSTF, however, recommends against routine use of these medications for women who are not at high risk for breast cancer, because the potential benefit is much smaller. Women who are over age 35 and are at high risk for breast cancer or who have had previous benign breast lesions (such as atypical ductal or lobular hyperplasia or lobular carcinoma in situ) might want to discuss this recommendation with their doctor. The USPSTF encouraged doctors to weigh the risk of breast cancer against potential drawbacks of the medications and the individual woman's risk for adverse effects.
Image: ShutterOK/Getty Images
Suffering from "chemo brain"? There's hope and many things you can do
Over the past decade, research has revealed that the majority of patients treated for cancer experience difficulties with memory, attention, concentration, and thinking. There are several lifestyle actions that can help improve these symptoms, as well as certain medications.

5 timeless habits for better health

What are the symptoms of prostate cancer?

Is your breakfast cereal healthy?

When pain signals an emergency: Symptoms you should never ignore

Does exercise give you energy?

Acupuncture for pain relief: How it works and what to expect

How to avoid jet lag: Tips for staying alert when you travel

Biofeedback therapy: How it works and how it can help relieve pain

Best vitamins and minerals for energy

Should you take probiotics with antibiotics?
Free Healthbeat Signup
Get the latest in health news delivered to your inbox!
Sign Up