5 timeless habits for better health

What are the symptoms of prostate cancer?

Is your breakfast cereal healthy?

When pain signals an emergency: Symptoms you should never ignore

Does exercise give you energy?

Acupuncture for pain relief: How it works and what to expect

How to avoid jet lag: Tips for staying alert when you travel

Biofeedback therapy: How it works and how it can help relieve pain

Best vitamins and minerals for energy

Should you take probiotics with antibiotics?
Diseases & Conditions Archive
Articles
Red, brown, green: Urine colors and what they might mean
Departures from the familiar yellow color of urine are often harmless but should be discussed with a doctor.
Most of the time, urine is a pale-yellow color because it contains urochrome, one of the substances produced when hemoglobin gets broken down. Hemoglobin is the protein in red blood cells that sticks to oxygen so it can be ferried around the body.
Occasionally, though, urine turns a very different color. Men may notice the change as their urine enters the toilet bowl or urinal. Women may be more likely to observe it after wiping. Seeing red or orange instead of the usual yellow can be alarming, especially if there are also symptoms like a burning sensation or pain with urination. The alarm may be justified: an abnormal urine color can be an early sign of a serious medical condition. To be on the safe side, it should be discussed with a doctor or another clinician.
Are varicose veins a health risk?
Ask the doctors
Q. I have a lot of varicose veins. Do they present any sort of a health risk?
A. Varicose veins are typically viewed as a mild, non-life-threatening condition that is more of a cosmetic annoyance than a serious health problem. That said, varicose veins can be associated with some health-related issues, such as swelling in the legs, blood clots, or damage to the skin caused by pressure from the veins. They may also make you more prone to skin damage, infections, and ulcers.
Allergic rhinitis: Your nose knows
Allergic rhinitis, commonly called hay fever, can be a minor seasonal nuisance or a troubling year-round problem. Most people can find relief by taking an antihistamine and by avoiding the allergens that trigger the irritation.
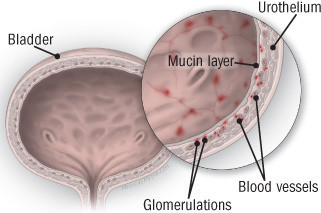
Diagnosing and treating interstitial cystitis
Also called painful bladder syndrome, this frustrating disorder disproportionately affects women.
Interstitial cystitis is a chronic bladder condition that causes recurring bouts of pain and pressure in the bladder and pelvic area, often accompanied by an urgent and frequent need to urinate — sometimes as often as 40, 50, or 60 times a day, around the clock. Discomfort associated with interstitial cystitis can be so excruciating that, according to surveys, only about half of people with the disorder work full-time. Because symptoms are so variable, experts today describe interstitial cystitis as a member of a group of disorders collectively referred to as interstitial cystitis/painful bladder syndrome. (In this article, we'll call it interstitial cystitis, or IC.)
Among the one to two million Americans with IC, women outnumber men by as much as eight to one, and most are diagnosed in their early 40s. Several other disorders are associated with IC, including allergies, migraine, irritable bowel syndrome, fibromyalgia (a condition causing muscle pain), chronic fatigue syndrome, and vulvodynia (pain or burning in the vulvar area that isn't caused by infection or skin disease).
How to talk to teens about the new coronavirus
Should I take blood pressure medications at night?
Ask the doctor
Q. I've taken blood pressure medicines every morning for many years, and they keep my pressure under control. Recently, my doctor recommended taking them at bedtime, instead. Does that make sense?
A. It actually does make sense — based on recent research. For many years, there have been at least three theoretical reasons for taking blood pressure medicines before bedtime. First, a body system that strongly affects blood pressure, called the renin-angiotensin system, has its peak activity during sleep. Second, circadian rhythms cause differences in the body chemistry at night compared with daytime. Third, most heart attacks occur in the morning, before medicines taken in the morning have a chance to "kick in."
Is osteoarthritis reversible?
Ask the doctors
Q. I recently started experiencing a lot of pain in my hand from osteoarthritis. Can I reverse this condition?
A. You can't reverse osteoarthritis, but there are things you can do to manage your pain and improve your symptoms. Osteoarthritis occurs when the protective cartilage that acts as cushioning between your bones starts to fray and wear down over time. Eventually this enables the bones to rub together, which causes the pain you are experiencing as well as swelling and stiffness that makes it difficult to move your hand freely. Typically, when you have arthritis, the pain and symptoms will be worse at some times than at others. You may experience a flare-up one day and feel better the next. To help reduce the discomfort of a flare-up, talk to your doctor about medication to relieve pain. She or he may recommend an over-the-counter pain reliever. Some people also get symptom relief using a topical pain reliever that is rubbed into the skin. Other strategies that can ease pain are splints or braces, heat or cold therapy, activity modification, and exercises or physical therapy to increase flexibility and strengthen your hand muscles.
Drooping Eyelid (Ptosis)
What Is It?
A drooping eyelid is also called ptosis or blepharoptosis. In this condition, the border of the upper eyelid falls to a lower position than normal. In severe cases, the drooping eyelid can cover all or part of the pupil and interfere with vision.
Ptosis can affect one or both eyes. It may be present at birth (congenital ptosis), or it may develop gradually over decades. Sometimes ptosis is an isolated problem that changes a person's appearance without affecting vision or health. In other cases, however, it can be a warning sign that a more serious condition is affecting the muscles, nerves, brain or eye socket. Ptosis that develops over a period of days or hours is more likely to signify a serious medical problem.
Ex-smokers are not free from long-term lung damage
In the journals
People who quit smoking decades ago are still at risk for lung diseases like chronic obstructive pulmonary disease (COPD), according to a study published online Oct. 9, 2019, by The Lancet Respiratory Medicine.
Researchers looked at lung capacity — the amount of air in your lungs after taking a deep breath — among more than 25,000 people and analyzed the results based on whether the individuals smoked, had quit smoking, or had never smoked. Previous research has suggested that the decline in lung capacity that occurs with smoking levels off within a few years after people quit.

5 timeless habits for better health

What are the symptoms of prostate cancer?

Is your breakfast cereal healthy?

When pain signals an emergency: Symptoms you should never ignore

Does exercise give you energy?

Acupuncture for pain relief: How it works and what to expect

How to avoid jet lag: Tips for staying alert when you travel

Biofeedback therapy: How it works and how it can help relieve pain

Best vitamins and minerals for energy

Should you take probiotics with antibiotics?
Free Healthbeat Signup
Get the latest in health news delivered to your inbox!
Sign Up