Heart disease and depression: A two way street
Learn ways to overcome the roadblocks that underlie these common and often-overlapping conditions.
- Reviewed by Christopher P. Cannon, MD, Editor in Chief, Harvard Heart Letter; Editorial Advisory Board Member, Harvard Health Publishing

Everyone feels sad, gloomy, or down in the dumps from time to time. But if those feelings linger for weeks and you start feeling hopeless, worthless, or just empty and numb, you may have depression. Like heart disease, depression is common, so it’s not unusual to have both conditions together.
But many people aren’t aware of the bidirectional connection between the two, says Dr. Stephanie Collier, director of education in the Division of Geriatric Psychiatry at Harvard-affiliated McLean Hospital. “A heart disease diagnosis may trigger a bout of depression. But having depression can also leave you more vulnerable to heart disease,” she says (see “A heavy heart”).
Some of the overlap stems from shared lifestyle factors, such as inactivity and an unhealthy diet. Addressing those issues may benefit both your mood and your heart. Other safe and effective ways to ease the burden of depression include working with a therapist and using a light box, options that are both now easier to access than they used to be. In addition to these strategies, there are many medications available for treating depression.
A heavy heartDepression affects the entire body, not just the brain. Like anxiety and stress, depression can be triggered by challenging life circumstances. The resulting boost in stress hormones can cause your blood pressure and heart rate to rise. Depression also appears to increase inflammation, a known culprit in the buildup of cholesterol-filled plaque in the arteries. In addition, it causes blood cell fragments known as platelets to become more “sticky” and likely to form clots in the bloodstream. This cascade of changes conspire to make a heart attack more likely. |
Be more active
Depression often leaves people listless, tired, and unmotivated, so the oft-heard advice to “just do some exercise” may not feel possible. But any activity is better than staying in bed, says Dr. Collier. Choose something you enjoy when you’re feeling well, even if it’s just going to a coffee shop. Once you’re out of the house, take a short walk. Next time, walk a little farther, she suggests. Spending time in nature can also help lighten your mood.
Eat well
Compared to the well-known connection between diet and heart health, the link between diet and mood isn’t as well established. Still, many of Dr. Collier’s patients are worried about dementia. “So I remind them that anxiety and depression can affect cognitive function and memory,” she says. Because they’re motivated to protect their brain health, they’re more receptive to improving their diets. Her three main tips: Cut back on meat, eat more vegetables (especially leafy greens), and replace less-healthy sources of fat (like butter) with olive oil.
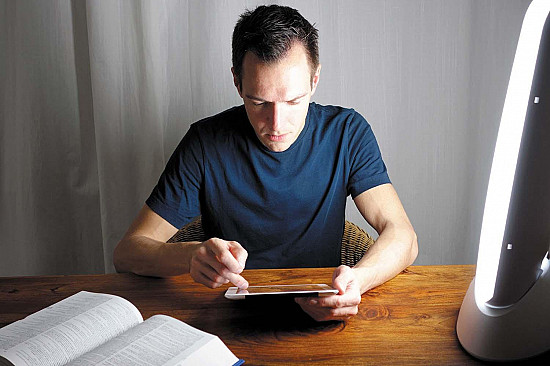
See the light
Although best known for treating seasonal depression, light therapy may also be an effective supplementary treatment for other types of depression, says Dr. Collier. You need to purchase or rent a light box that emits 10,000 lux (a measure of light intensity) and sit in front of the light for about 30 minutes every morning, as soon as possible after you wake up. To make sure you’re getting an effective product, check the Center for Environmental Therapeutics, a nonprofit organization that provides advice for selecting a light box.
Talk it out
Finding a therapist is now far easier than in the past, thanks to online platforms such as Alma, Headway, and others that connect people with therapists who take their insurance. “Since COVID, when therapy went online, the landscape has really changed,” says Dr. Collier. For therapy, telehealth visits are more convenient and just as effective as in-person sessions. “Sometimes, people are more willing to share details about themselves when they’re on a screen than in person,” says Dr. Collier.
Medication guidance
Medications aren’t recommended for mild to moderate depression because the episodes usually resolve on their own, especially if you embrace the other interventions described above, says Dr. Collier. While only about 30% to 40% of people who take antidepressants notice a meaningful improvement, these drugs remain important tools for many people. Cardiologists tend to recommend the antidepressant sertraline (Zoloft) because it has fewer known heart-related side effects than related drugs, known collectively as SSRIs, says Dr. Collier. Of note: In older adults, high doses of another popular SSRI, citalopram (Celexa), can raise the risk of a serious heart rhythm disorder (see “What is long QT syndrome?” in the May 2018 Heart Letter). People over 60 should not take citalopram in doses higher than 20 milligrams.
This article is brought to you by HarvardHealthOnline+, the trusted subscription service from Harvard Medical School. Subscribers enjoy unlimited access to our entire website, including exclusive content, tools, and features available only to members. If you're already a subscriber, you can access your library here.
Image: © Hispanolistic/Getty Images
About the Author

Julie Corliss, Executive Editor, Harvard Heart Letter
About the Reviewer

Christopher P. Cannon, MD, Editor in Chief, Harvard Heart Letter; Editorial Advisory Board Member, Harvard Health Publishing
Disclaimer:
As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician.